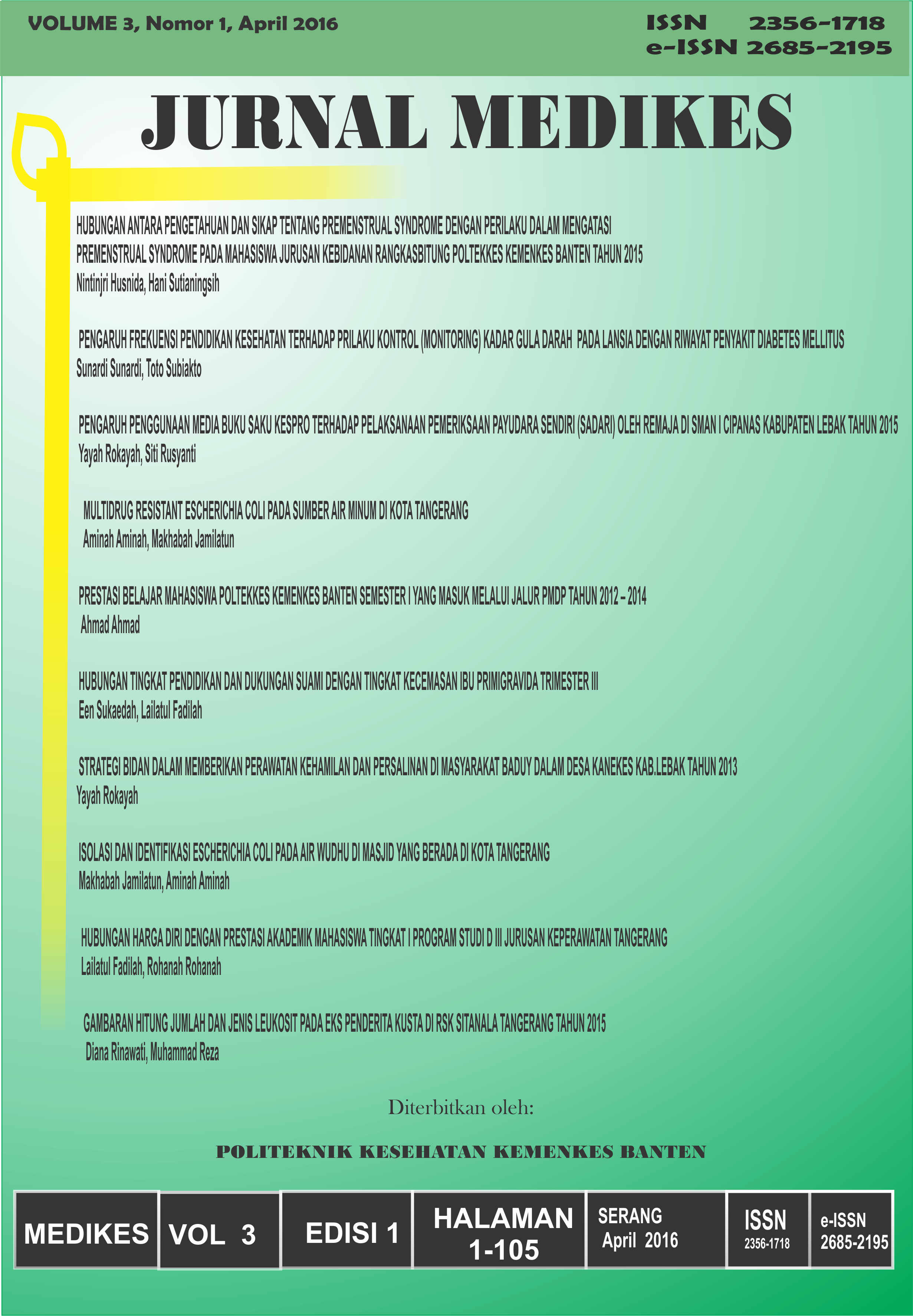
MULTIDRUG RESISTANT ESCHERICHIA COLI PADA SUMBER AIR MINUM DI KOTA TANGERANG
DOI:
https://doi.org/10.36743/medikes.v3i1.150Keywords:
Multidrug resistance, E. coli, Air MinumAbstract
Multidrug-resistant Escherichia coli (MDR E. coli) telah menjadi perhatian dalam hal kesehatan masyarakat di berbagai negara. Bakteri ini menyebabkan infeksi yang sulit ditangani sehingga dampak buruk yang ditimbulkan bagi kesehatan menjadi luas. Penelitian ini bertujuan untuk menentukan prevalensi dan kerentanan MDR E. coli yang diisolasi dari sumber air minum masyarakat yang berada di Kota Tangerang. Penelitian ini dilaksanakan pada bulan Mei – Juni 2015. Desain yang digunakan adalah penelitian eksperimental laboratorium. Populasi dalam penelitian ini adalah seluruh bakteri E. coli yang diisolasi dari sumber air minum masyarakat di Kota Tangerang. Semua bakteri yang diisolasi digunakan sebagai sampel. Hasil penelitian menunjukkan bahwa dari 16 sumber air minum masyarakat, enam di antaranya positif mengandung E. coli dan satu sumber air minum positif mengandung MDR E. coli. Oleh karena itu untuk mencegah masalah kesehatan yang lebih jauh, perlu dilakukan pemeriksaan berkala terhadap berbagai bakteri patogen yang ada di masyarakat.
References
2. Drago, L., et al., In vitro selection of resistance in Escherichia coli and Klebsiella spp. at in vivo fluoroquinolone concentrations. BMC Microbiol, 2010. 10: p. 119.
3. Bartoloni, A., et al., Multidrug-resistant commensal Escherichia coli in children, Peru and Bolivia. Emerg Infect Dis, 2006. 12(6): p. 907-13.
4. Sahm, D.F., et al., Multidrug-resistant urinary tract isolates of Escherichia coli: prevalence and patient demographics in the United States in 2000. Antimicrob Agents Chemother, 2001. 45(5): p. 1402-6.
5. Liebana, E., et al., Public health risks of enterobacterial isolates producing extended-spectrum beta-lactamases or AmpC beta-lactamases in food and food-producing animals: an EU perspective of epidemiology, analytical methods, risk factors, and control options. Clin Infect Dis, 2013. 56(7): p. 1030-7.
6. Magiorakos, A.P., et al., Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect, 2012. 18(3): p. 268-81.
7. Howard, D.H., et al., The global impact of drug resistance. Clin Infect Dis, 2003. 36(Suppl 1): p. S4-10.
8. Coates, A., et al., The future challenges facing the development of new antimicrobial drugs. Nat Rev Drug Discov, 2002. 1(11): p. 895-910.
9. Peralta, G., et al., Impact of antibiotic resistance and of adequate empirical antibiotic treatment in the prognosis of patients with Escherichia coli bacteraemia. J Antimicrob Chemother, 2007. 60(4): p. 855-63.
10. Rahman, S., et al., Antibacterial activity of natural spices on multiple drug resistant Escherichia coli isolated from drinking water, Bangladesh. Ann Clin Microbiol Antimicrob, 2011. 10: p. 10.
11. Guerra, B., et al., Phenotypic and genotypic characterization of antimicrobial resistance in Escherichia coli O111 isolates. J Antimicrob Chemother, 2006. 57(6): p. 1210-4.
12. Boyd, L.B., et al., Increased fluoroquinolone resistance with time in Escherichia coli from >17,000 patients at a large county hospital as a function of culture site, age, sex, and location. BMC Infect Dis, 2008. 8: p. 4.
13. Kibret, M. and B. Abera, Antimicrobial susceptibility patterns of E. coli from clinical sources in northeast Ethiopia. Afr Health Sci, 2011. 11 Suppl 1: p. S40-5.
14. Kader, A.A. and A.K. Kumar, Prevalence of extended spectrum beta-lactamase among multidrug resistant gram-negative isolates from a general hospital in Saudi Arabia. Saudi Med J, 2004. 25(5): p. 570-4.
15. Poespoprodjo, J.R., et al., Dihydroartemisinin-piperaquine treatment of multidrug resistant falciparum and vivax malaria in pregnancy. PLoS One, 2014. 9(1): p. e84976.
16. Marwoto, et al., Correlation of Single Nucleotide Polymorphism 35-Kb Upstream of HLA-C and Clinical Profile of Multidrug-Resistant Tuberculosis. J Clin Diagn Res, 2015. 9(9): p. DC10-3.
17. Wong, V.K., et al., Phylogeographical analysis of the dominant multidrug-resistant H58 clade of Salmonella Typhi identifies inter- and intracontinental transmission events. Nat Genet, 2015. 47(6): p. 632-9.
18. Waturangi, D.E., et al., Edible ice in Jakarta, Indonesia, is contaminated with multidrug-resistant Vibrio cholerae with virulence potential. J Med Microbiol, 2013. 62(Pt 3): p. 352-9.
19. Pfaller, M.A., et al., Candida krusei, a multidrug-resistant opportunistic fungal pathogen: geographic and temporal trends from the ARTEMIS DISK Antifungal Surveillance Program, 2001 to 2005. J Clin Microbiol, 2008. 46(2): p. 515-21.
20. Maeda, S., et al., Multidrug resistant Mycobacterium leprae from patients with leprosy. Antimicrob Agents Chemother, 2001. 45(12): p. 3635-9.
21. Toshima, H., et al., Detection and isolation of Escherichia coli with a coding gene for enteroaggregative Escherichia coli heat-stable enterotoxin 1 from food and comparison with fecal isolates. J Food Prot, 2004. 67(10): p. 2117-22.
22. Janezic, K.J., et al., Phenotypic and Genotypic Characterization of Escherichia coli Isolated from Untreated Surface Waters. Open Microbiol J, 2013. 7: p. 9-19.
23. Baquero, F. and J. Blazquez, Evolution of antibiotic resistance. Trends Ecol Evol, 1997. 12(12): p. 482-7.
24. Lipsitch, M. and M.H. Samore, Antimicrobial use and antimicrobial resistance: a population perspective. Emerg Infect Dis, 2002. 8(4): p. 347-54.
25. Thomas, C.M. and K.M. Nielsen, Mechanisms of, and barriers to, horizontal gene transfer between bacteria. Nat Rev Microbiol, 2005. 3(9): p. 711-21.
26. Furuya, E.Y. and F.D. Lowy, Antimicrobial-resistant bacteria in the community setting. Nat Rev Microbiol, 2006. 4(1): p. 36-45.
27. Hughes, V.M. and N. Datta, Conjugative plasmids in bacteria of the 'pre-antibiotic' era. Nature, 1983. 302(5910): p. 725-6.
28. Shin, S.W., et al., Prevalence of Antimicrobial Resistance and Transfer of Tetracycline Resistance Genes in Escherichia coli Isolates from Beef Cattle. Appl Environ Microbiol, 2015. 81(16): p. 5560-6.
29. Cerquetti, M., et al., Ciprofloxacin-resistant, CTX-M-15-producing Escherichia coli ST131 clone in extraintestinal infections in Italy. Clin Microbiol Infect, 2010. 16(10): p. 1555-8.
30. Falagas, M.E., et al., Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum beta-lactamase producing, Enterobacteriaceae infections: a systematic review. Lancet Infect Dis, 2010. 10(1): p. 43-50.
31. Oteo, J., et al., Parallel increase in community use of fosfomycin and resistance to fosfomycin in extended-spectrum beta-lactamase (ESBL)-producing Escherichia coli. J Antimicrob Chemother, 2010. 65(11): p. 2459-63.
32. Falagas, M.E., et al., Fosfomycin versus other antibiotics for the treatment of cystitis: a meta-analysis of randomized controlled trials. J Antimicrob Chemother, 2010. 65(9): p. 1862-77.
33. Galatti, L., et al., Antibiotic prescribing for acute and recurrent cystitis in primary care: a 4 year descriptive study. J Antimicrob Chemother, 2006. 57(3): p. 551-6.
34. Knottnerus, B.J., et al., Fosfomycin tromethamine as second agent for the treatment of acute, uncomplicated urinary tract infections in adult female patients in The Netherlands? J Antimicrob Chemother, 2008. 62(2): p. 356-9.
35. Oteo, J., et al., CTX-M-15-producing urinary Escherichia coli O25b-ST131-phylogroup B2 has acquired resistance to fosfomycin. J Antimicrob Chemother, 2009. 64(4): p. 712-7.
Downloads
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.